Vitamin D supplements aren’t living up to their hype
Recent studies say taking extra amounts of the nutrient may not be a boon for every body
DISCOURAGING Testing for vitamin D deficiency is way up in the United States, but recent studies find that supplements of the nutrient may do less than expected.
Jeff Rogers
In the supplement world, vitamin D is a bit like a Kardashian. Its fame seemed to come out of nowhere about a decade ago, garnering so much press so fast that it’s hard to remember a time when people weren’t talking about it.
Vitamin D had long been known for protecting bones, but its star began to rise in the early 2000s after researchers made connections hinting that vitamin D was good for a lot more than our skeletons. It appeared to help protect against a lengthy list of ailments, including multiple sclerosis, asthma, depression, heart disease and cancer. The vitamin also was said to improve athletic performance.
Organizations like the Vitamin D Council — the 2003 brainchild of a psychiatrist who became a vitamin D enthusiast — began to actively promote the benefits to the public and to physicians, while selling test kits for vitamin D blood levels. Doctors checked for it; patients demanded testing. Researchers latched on.
But with more research comes more scrutiny, and most recently, a series of seemingly tarnishing findings. On November 10, the New England Journal of Medicine published the largest study so far to test vitamin D supplements’ protection against cancer and heart disease. The results were generally interpreted as inconclusive at best and disappointing at worst. One 2017 review of the evidence for cardiovascular benefits concluded that studies of people taking vitamin D “have failed to show clear improvements in blood pressure, insulin sensitivity or lipid parameters.”
Even the vitamin’s reputation for helping bones took a hit last April from the U.S. Preventive Services Task Force. The independent group, which makes health policy recommendations, concluded that when it comes to preventing fractures, there is not enough evidence to recommend for or against supplementation (except for postmenopausal women, who get no benefit from taking vitamin D supplements of 400 international units, or IUs, or less).
Today, enthusiasm for the vitamin, at least in scientific circles, is fading, says Clifford Rosen, an osteoporosis researcher at the Maine Medical Center Research Institute in Scarborough. “I think even in the bone world, where we know vitamin D may have some effect, the studies aren’t very compelling.” Which leads to the question: Is the sun finally setting on vitamin D?
Does a body good?
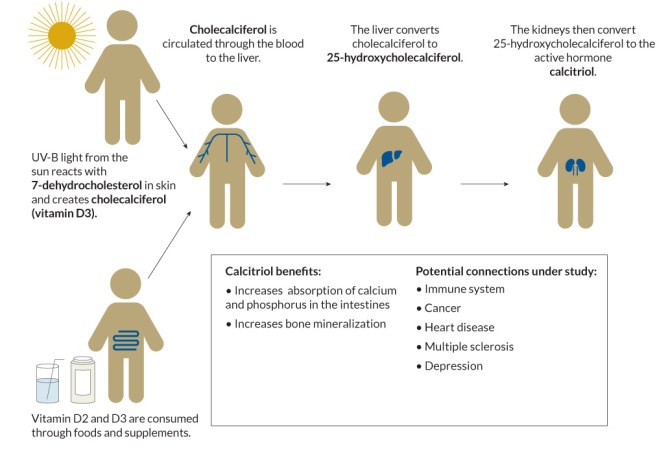
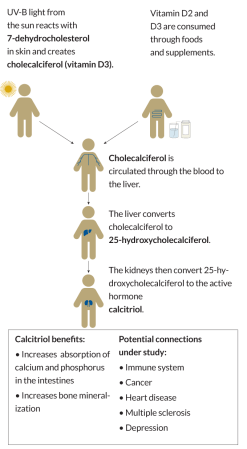
The body makes vitamin D when exposed to ultraviolet light, or absorbs it from food. Once in the bloodstream, vitamin D undergoes several transformations into a hormone that helps strengthen bones. Research showing its effects on other organs is coming up short.
Shining a light
The answer, as with most matters of nutrition, is complicated.
One thing is indisputable: The body must have vitamin D. Throughout most of human history, rickets was a feared childhood disease. As babies became toddlers, their legs and arms would sometimes bend like willow branches. Even affluence offered no protection: Some victims were the sons and daughters of the Medici family, the powerful dynasty of the Italian Renaissance. Finally, in the early 1900s, doctors figured out the cause — insufficient sun. In 1919, a German doctor showed that rickets could be treated by exposing an affected arm to ultraviolet lamps. Remarkably, sun exposure on one arm healed both.
The cure came not from sunshine itself, but from vitamin D, an essential chemical that the body makes in the presence of UV light. For discovering the mechanism of vitamin D formation, German chemist Adolf Windaus won a Nobel Prize in 1928. Over the following decades, foods were increasingly fortified and rickets gradually disappeared in most places. Vitamin D became little more than a mention on milk cartons and bottles of orange juice.
In the body, this essential nutrient travels a convoluted path, starting with a substance in the skin called 7-dehydrocholesterol. In the presence of sunlight, that chemical is transformed into vitamin D, or cholecalciferol, and enters the bloodstream. When it reaches the liver, vitamin D is converted into another chemical, 25-(OH)D, or 25-hydroxycholecalciferol. In the kidneys and other organs, 25-(OH)D changes into the active form of vitamin D, called calcitriol. Calcitriol, a hormone, is so named because it encourages calcium absorption through the wall of the intestine into the bloodstream.
Vitamin D’s primary job is to help the body absorb calcium from food. Rickets occurs when bones are starved of calcium. Vitamin D also aids in the uptake of phosphorus, another bone-strengthening nutrient.
“For a long time, it was thought the benefit was mainly on bone health,” says Walter Willett, an epidemiologist and nutrition researcher at the Harvard T.H. Chan School of Public Health. Then scientists began to discover that a broad array of tissues contain proteins that serve as welcome mats for the vitamin. “There were receptors for vitamin D in almost every organ in the body, not just in bones,” Willett says. “What was vitamin D doing in places other than bone?”
By the late 1990s, scientists were finding links between low sunlight exposure and a variety of diseases, some of them surprising. Several studies noted that the farther north a person lived — a proxy for less intense sun — the higher the risk of multiple sclerosis and other autoimmune conditions. In one early study, published in Cancer Epidemiology, Biomarkers and Prevention, women who lived in the sunnier parts of the United States had breast cancer rates that were 25 percent to as much as 65 percent lower than women who lived farther north. Another study that made headlines in 2008, from Archives of Internal Medicine, reported that Americans in the lower quarter of vitamin D blood levels had a 26 percent higher chance of death over the nine years studied than those with the highest levels of vitamin D.
In other words, a lot of early research suggested that people with abundant vitamin D — or at least with the best chances of sun exposure — appeared to be healthier. Problem is, there may be other reasons that less sun correlates with certain diseases, says JoAnn Manson, chief of preventive medicine at Harvard-affiliated Brigham and Women’s Hospital in Boston. People may not be going outdoors because they are ill, for example, or less inclined to exercise.
The amount of sun “may not be causally related in any way to these health outcomes,” Manson says. Or a low vitamin D blood level could be a consequence of obesity; the vitamin is soluble in fat, so it can become sequestered inside adipose tissue. The detriment to health may not be from low vitamin D directly, but from excess body weight, too little physical activity or other known influences on a person’s health.
The central question today is not whether the body needs vitamin D — it absolutely does — but whether the average person should be taking a supplement. There is widespread public belief that it’s a good idea. According to market research firm Euromonitor International, annual U.S. consumer spending on vitamin D has risen from $248 million in 2008 to more than $1 billion today.
$248millionU.S. consumer spending on vitamin D in 2008 |
|
$1billionU.S. consumer spending on vitamin D today |
One of the first randomized controlled trials to study vitamin D supplementation, by researchers at Creighton University in Omaha, Neb., was published in 2007. In that study, 1,179 women over age 55 were randomly assigned to take about 1,500 milligrams daily of calcium, calcium plus 1,100 IUs of vitamin D (that’s about twice the recommended dietary allowance, or RDA), or a placebo. Writing in the American Journal of Clinical Nutrition, the researchers reported a dramatically lower (more than 50 percent) cancer incidence after four years among the women in the vitamin D with calcium group compared with those who took a placebo — at least when the results analyzed women who had stayed in the study for a year or more. There were 18 cancers diagnosed after the second year in the placebo group compared with eight among women who took calcium plus vitamin D. The finding made sense because around this time, a growing number of laboratory studies demonstrated that the vitamin had anticancer properties in lab animals.
“People tended to glom on to positive results because they wanted them to be true,” says Steven Abrams, a pediatrician at the University of Texas at Austin and a member of a 2010 Institute of Medicine panel that evaluated vitamin D (SN: 7/16/11, p. 22). “Negative studies were buried, harder to find.”
In 2010, a headline in the New York Times read, “Vitamin D, Miracle Drug: Is It Science, or Just Talk?” The story described a clinical trial named VITAL that was just starting at Brigham and Women’s Hospital, with Manson as one of the study leaders. At almost 26,000 participants, VITAL would become the largest randomized trial to measure whether men over 50 and women over 55 who took a daily vitamin D supplement of 2,000 IUs were protected from cancer and heart disease. (The study also tested fish oil supplements.) Importantly, more than 5,000 volunteers were African-American. People with darker skin may have a harder time making vitamin D in sunlight because they don’t absorb as much UV light, the driver of vitamin D formation. VITAL became one of the most anticipated vitamin D studies.
D-flating news
VITAL trial results were released in November in Chicago at the American Heart Association’s annual scientific sessions and published in the New England Journal of Medicine. Fish oil supplements offered some benefits, preventing heart attacks, but not stroke. Extra vitamin D offered no heart protection (SN: 12/8/18, p. 9).
People tended to glom on to positive results because they wanted them to be true.
— Steven Abrams
As for cancer prevention, the study produced “a complex finding,” Manson says. Over the entire five years, there was no reduction in the risk of being diagnosed with breast, prostate or colon cancer, but the overall risk of dying from cancer was slightly lower. In all, 154 deaths from cancer occurred in the vitamin D group versus 187 in the placebo group. When the analysis was narrowed to those who were in the trial for at least two years, the researchers saw a 25 percent reduction in death from cancer with vitamin D. Perhaps vitamin D makes tumors less likely to grow and spread, Manson says. If that’s true, any benefit would take time to appear. “This warrants further study,” she says.
The VITAL results were the latest of a string of largely discouraging news. In 2017, scientists had reported the results of a study testing whether monthly high doses of vitamin D could prevent heart problems. About 5,000 people from the general population of New Zealand were randomly assigned to receive the vitamin D boost or a placebo. In JAMA Cardiology, the researchers reported that supplementation made no difference.
As a safeguard against bone fractures, vitamin D has not fared much better. Because the vitamin is necessary for bone health, many doctors recommend supplements for older people to help prevent breaks and falls. Yet the U.S. Preventive Services Task Force concluded last spring that the evidence for this advice was still inconclusive. Another blow came in October, when researchers reported in Lancet Diabetes and Endocrinology that a review and summary of studies so far “suggest that vitamin D supplementation does not prevent fractures or falls, or have clinically meaningful effects on bone mineral density.”
Sunshine on my shoulder

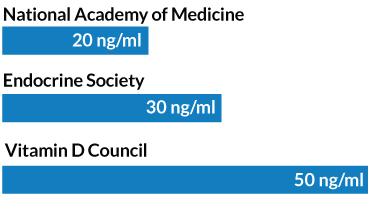
The National Academy of Medicine advises a vitamin D intake of 600 to 800 international units per day to achieve blood levels of 20 nanograms/milliliter of the nutrient (one of the lower recommended thresholds). To make enough from the sun, depending on the latitude and season, about 10 minutes outside in shorts and a T-shirt will do for a light-skinned person. People with darker skin need more time.
Recommended minimal vitamin D blood level
That’s not as surprising as it may seem, even given vitamin D’s claim to fame in bone health, says Catharine Ross, a nutritional biochemist at Penn State who chaired the 2010 vitamin D panel. Bone is built early in life, she says. Later in life, the body works to preserve that bone. Much of that preservation isn’t orchestrated by vitamin D itself, but by the hormone calcitriol, whose production is limited by the liver and kidneys. In other words, more vitamin D on the front end doesn’t necessarily mean more of the hormone on the back end.
The news for cancer from studies other than VITAL has also been inconsistent. On the supportive side of the ledger, a compilation of studies on colorectal cancer, published last June in the Journal of the National Cancer Institute, found a clear elevation in risk for people with the lowest blood levels of the vitamin. People who had a vitamin D blood level below 12 nanograms per milliliter had a colorectal cancer risk 31 percent higher over five years than those whose blood levels were twice as high.
Yet a 2017 study found that the big reduction in cancer incidence announced in 2007 by Creighton University researchers didn’t hold up. In contrast to the 2007 trial, this one, reported in JAMA by many of the same Creighton researchers, found no difference in cancer risk among postmenopausal women who took vitamin D and calcium and those who took a placebo.
Overall, “there have been enough systematic reviews and large randomized controlled trials suggesting that vitamin D does not have an effect in the primary prevention of cancer,” says Cindy Davis, director of grants and extramural activities at the Office of Dietary Supplements, part of the National Institutes of Health. She names a long list of groups that have looked at the research, including the Institute of Medicine (now the National Academy of Medicine), the Agency for Healthcare Research and Quality, the U.S. Preventive Services Task Force and the World Cancer Research Fund International.
“They’ve all said that there’s not enough evidence, or that the evidence suggests that vitamin D supplementation does not appear to be protective” against cancer formation, Davis says.
But Willett, the Harvard nutrition expert, thinks studies so far have been too short to meaningfully address the cancer question. Most tumors unfold quietly over decades, so even a five-year study might not be long enough. It would take a decade or more for solid answers. “People can smoke for 20 years and there’s no effect on cancer risk,” he says. He points to the recent colorectal cancer review suggesting a big reduction in risk with higher blood levels of vitamin D. “If that was a drug, it would be a blockbuster.”
He also says that there are diseases, such as multiple sclerosis, that have held up over time as being associated with sunlight or vitamin D. One of the latest studies appeared in April in Neurology. Researchers from Harvard and the University of British Columbia in Vancouver measured the risk of multiple sclerosis across a lifetime of sun exposure. People who lived in areas with the highest amounts of UV light had a 45 percent lower risk of the disease than those who lived in areas with the lowest sun exposure, and the protection appeared to be much more pronounced among people who reported high summer sun in childhood and adolescence.
Studies are now testing whether adding various doses of vitamin D to regular treatments can help people with MS. Other studies are testing prevention or treatment of asthma, diabetes and depression.
Help for MS
Evidence that vitamin D might help protect against multiple sclerosis has been building. One recent report found generally higher death rates from MS in northern U.S. states, where sunlight is less intense and winter days are shorter, compared with southern states. (In the graph below, a few states are excluded because of low population numbers.) Researchers are now testing whether vitamin D supplementation added to MS treatment might help people with the disease.
Multiple sclerosis deaths in U.S. states by latitude
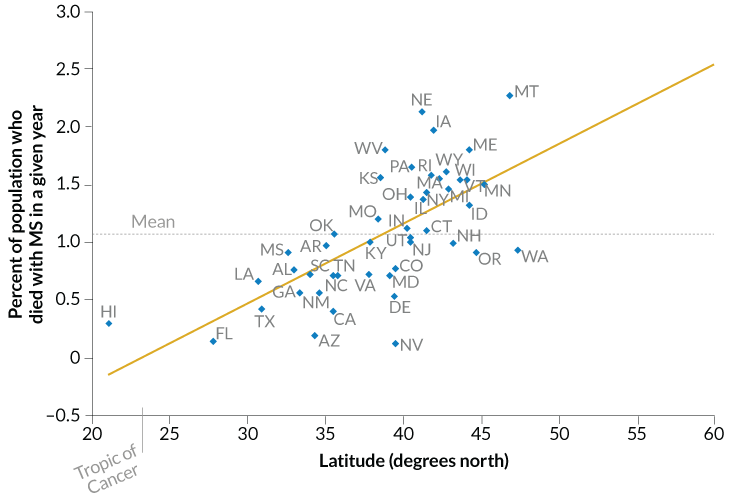
Source: G.E. Davis and W.E. Lowell/J. Photochem. and PhotobioL. B: Biol. 2015
Testing tumult
Judging by the market, millions of health-conscious consumers aren’t waiting for science to work everything out. Some researchers worry that promotion of vitamin D has created a misguided “more is better” mind-set. At high doses, “there are some studies that do show harm,” says Davis, of the NIH Office of Dietary Supplements. Participants in the VITAL study, which included a daily dose of 2,000 IUs, did not appear to have any major side effects. But some pills are sold at much higher amounts, as high as 50,000 IUs to be taken weekly.
And some pills contain the less-accessible form of vitamin D produced by plants, called D2, not the version made by the human body, called D3. Nothing about vitamin D is simple. Its effects probably have a U-shaped curve for some diseases, Davis says. Too little or too much in the bloodstream can be harmful, but most levels in the middle are fine.
Testing bonanza
With growing publicity on potential health benefits of vitamin D, testing for the nutrient surpassed testing for other nutrients in older Americans after 2008.
Blood testing for various nutrients
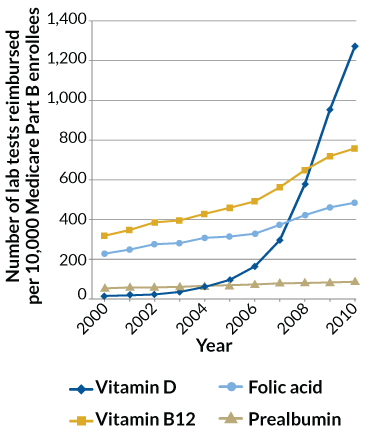
Source: S. Shahangian et al/Arch. Pathol. Lab. Med. 2014
One paper published in 2018 in Cancer Research examined 19 studies of vitamin D’s association with prostate cancer. That analysis found that higher levels of vitamin D were associated with an increased risk of prostate cancer, although the researchers say this could be due to detection bias — perhaps the men with high vitamin D were more health conscious and more likely to get screened for the disease.
Which gets back to the thorny issue of whether it’s necessary to check your vitamin D levels, which can cost from around $50 to more than $100 if it’s not covered by insurance. Testing has grown exponentially, Willett says, yet “we still don’t know what target number we should be aiming for.”
Public health officials recommend blood levels above 20 ng/ml. The Endocrine Society, which represents doctors, states that some adults are deficient if their levels are below 30 ng/ml. Advocates like the Vitamin D Council set higher thresholds.
In addition to disagreement over a target number, there is controversy over which form of vitamin D to measure, and how to measure it. Davis says testing is tricky because the vitamin goes through several steps to get to its active form. The best marker of vitamin D status is 25-(OH)D, she says. That’s the form that the liver makes (not the kind that enters the bloodstream from the skin). But until recently there were no standards for measuring 25-(OH)D.
A 2017 report in the Journal of Steroid Biochemistry and Molecular Biology pointed out how results can vary from test to test: One method suggested a decline in vitamin D levels in the American population from the late 1980s to the early 2000s; another, testing blood from the exact same people, showed no change. Same samples, different test, different results. As the authors note, “the vitamin D field is in chaos.”
Results may vary
Controversy has surrounded vitamin D testing, which has lacked rigorous standards. Analysis by one method (left) suggested that vitamin D levels were falling among Americans. Yet a more standardized analysis of the same samples (right) showed very little difference.
Impact of standardizing blood testing for vitamin D
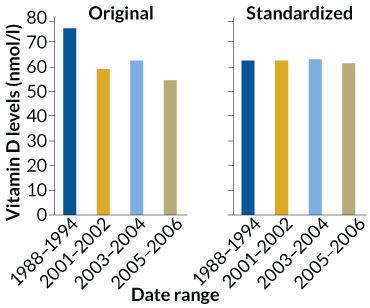
Source: N. Binkley et al/J. Steroid Biochem. Mol. Biol. 2017
Willett doesn’t see much value in focusing on blood test numbers. Even if you don’t know your exact levels, taking 1,000 or 2,000 IUs “is a reasonable thing to do,” he says, given studies finding that the level is safe and showing evidence of benefit against cancer death.
Rosen, from the Maine Medical Center, doesn’t think the supplements will make a dramatic difference in health, but agrees that a 2,000-IU supplement won’t do harm either. “When I go and talk to doctors I say, ‘How many [of you] are taking vitamin D?’ The hands go up,” he says. Most of them. When he asks why, the doctors respond, “ ‘Eventually it’s going to be proven that it prevents something.’ ” Belief in vitamin D runs deep.
That said, there are certain populations that doctors already know may need supplements to reach even minimally adequate levels: babies who are exclusively breastfed, some people with dark skin, some who live in northern latitudes and people who don’t have much exposure to daylight because they live in institutions such as nursing homes or hospitals.
Amid the uncertainty, clinicians are left to advise patients. By nature, researchers zero in on just a few specifics in their studies. “But the world isn’t like that. The world is very complicated,” says Dena Herman, a nutrition researcher at the UCLA Fielding School of Public Health. In the end, people have to consider their own personal circumstances, she says. Herman doesn’t immediately suggest supplements when a patient appears to have inadequate levels of vitamin D. Often these patients are overweight, which could be affecting their vitamin D levels. “I usually recommend they get more physically active and get in the sun first,” she says. “If people could master the basics, they wouldn’t have to worry about supplements.”