Virtual reality therapy has real-life benefits for some mental disorders
Cheap, user-friendly hardware could help VR therapy go mainstream

ERASING FEAR Confronting phobias, post-traumatic stress and other mental disorders may become possible for more people as virtual reality therapy goes mainstream.
Jamie Jacob
Edwin adjusted his headset and gripped the game controller in both hands. He swallowed hard. The man had good reason to be nervous. He was about to enter a virtual environment tailor-made to get his heart pumping way more than any action-packed video game: a coffee shop full of people.
Determined to overcome his persistent fear that other people want to hurt him, Edwin had enrolled in a study of a new virtual reality therapy. The research aimed to help people with paranoia become more comfortable in public places. In this program, described in March in the Lancet Psychiatry, Edwin could visit a store or board a crowded bus.
Virtual strangers can be scary, just like real people. Edwin, who had been diagnosed with paranoid schizophrenia, often found simple errands like grocery shopping overwhelming and exhausting.
But facing simulated crowds came with perks. At a nearby computer sat clinical psychologist Roos Pot-Kolder of VU University Amsterdam. She could customize the number of avatars and set their friendliness levels in each scene. That way, Edwin could progress at his own pace.
During one session, Pot-Kolder coached Edwin to challenge his own paranoid assumptions. If he saw an angry-looking avatar, she asked, “What could be other reasons for looking mad, besides wanting to hurt you?” Edwin offered: The person could be tired or having personal problems.
After three months of VR treatment, public outings were easier, said Edwin, who asked that his last name not be used. “I felt more freedom, more relaxed.” He even performed a poem for 500 people at a talent show, which he “would not have dared” before.
Researchers have been developing virtual reality systems that help people overcome specific phobias since the 1990s. VR therapy has since expanded to address more complex anxiety disorders, such as social anxiety and post-traumatic stress, and even the anxiety associated with paranoid schizophrenia for people like Edwin.
“The key ingredient to an effective treatment for anxiety disorders is … you need to face your fears,” says Stéphane Bouchard, a clinical cyberpsychologist at the University of Quebec in Outaouais, Canada. He’s referring to what’s known as exposure therapy. With emotional support from a therapist, exposure therapy helps desensitize the patient to whatever the fear is. Patients typically face their fears in real life or, if their fear is a traumatic memory, repeatedly relive the event in their imagination.
But confronting fears can be easier in a virtual setting. A flight-phobic patient can take off and land many times in a single VR session without the cost and hassle of actual flights. Veterans with post-traumatic stress who can’t remember a traumatic memory in great detail can reenact a close proxy in VR for a more potent therapeutic experience. The same goes for those who repress painful memories.
Until recently, the price and complexity of VR equipment, which could run tens of thousands of dollars, limited VR therapy to a few research labs and clinics. Now, there are computer-based headsets like the Oculus Rift that cost only a few hundred dollars, as well headsets such as the Samsung Gear VR that turn smartphones into virtual reality displays for about 100 bucks.
With cheaper, more user-friendly systems poised to make virtual reality therapy available to many more patients, researchers are testing the bounds of VR’s therapeutic powers to treat a broader range of disorders or, in some cases, replace the therapist altogether.
EXPOSURE THERAPY A VR system that helps people with paranoia get more comfortable in public places, such as a café or grocery store (shown in the clip above), uses avatars that can be made to look friendlier or more hostile, depending on a patient’s progress. |
Real feel
The power of VR therapy comes from the fact that people automatically react to fear cues, even in an environment they consciously know isn’t real. That’s because the brain’s emotional command center, or limbic system, responds to stressors in a matter of milliseconds — way faster than logic can kick in (SN: 2/26/11, p. 22).
As a result, patients who confront their fears in VR have shown increased levels of the stress hormone cortisol, higher heart rate and higher skin conductivity, says Barbara Rothbaum, a clinical psychologist at Emory University in Atlanta. Those are all telltale signs of a fight-or-flight response (SN Online: 2/2/17).
Back when Rothbaum and colleagues began to study VR treatment for a psychological disorder in the early 1990s, the researchers weren’t sure that a computer simulation could provoke those reactions. But their VR program, which took height-phobic patients onto bridges, balconies and for a ride in a glass elevator, worked almost too well.
Rothbaum recalls the very first patient test. “We were so excited, and she was getting anxious. We just kept her going in it, and she ended up throwing up.” The patient, it turned out, was susceptible to motion sickness — a problem that still plagues VR (SN: 3/18/17, p. 24). “We thought that was going to be the end of the study right there.”
But Rothbaum’s team forged ahead. The group learned to give patients a break after about 40 minutes in VR, dial the thermostat down and warn nausea-prone patients not to move their heads so much. In that first study, reported in 1995 in the American Journal of Psychiatry, 10 participants showed a substantial decrease in fear of heights after seven weekly sessions of VR therapy compared with seven patients who received no therapy. Two decades on, studies have shown that VR treatments for specific phobias can soothe people’s fears about as well as real-life exposure.
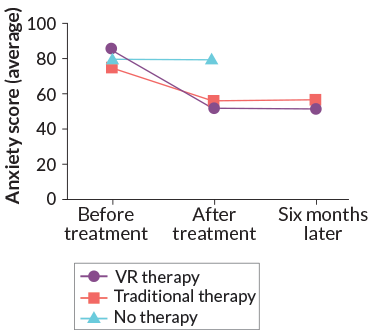
More recently, researchers have designed and tested VR systems to help people with more nuanced and diverse fear triggers, such as social anxiety or obsessive-compulsive disorder. For social anxiety, Bouchard and colleagues tested a VR system that allowed patients to work through tense social situations, such as a job interview or declining to purchase something from a persistent store clerk. The researchers assigned 17 socially anxious people to VR therapy and another 22 to typical exposure treatment that involved exercises like talking to strangers in public. A third group assigned to a waiting list got no therapy.
Before and after 14 weekly therapy sessions, participants reported their fear and avoidance of social situations from 0 to 144, with higher scores indicating more severe anxiety. Starting scores averaged between 75 and 85. Participants who got VR treatment dropped an average of 33 points, whereas real-life exposure participants dropped an average of 19. The no-treatment group stayed about the same. These results, reported in the April 2017 British Journal of Psychiatry, suggest that VR is at least as effective as real-life exposure for social anxiety.
Helping patients with post-traumatic stress disorder confront their fears is often more complex than simulating a generic high-rise or spider. One system that provides a broad menu of fear cues to patients with PTSD, created by VR therapy developer Albert “Skip” Rizzo and colleagues at the University of Southern California in Los Angeles, helps people suffering from post-traumatic stress after military duty in Iraq and Afghanistan.
To relive a traumatic memory in this VR system, the patient first chooses the setting, like a roadway checkpoint or a hospital. As the patient narrates the memory aloud, the therapist customizes the scene. If “the patient is saying, ‘I’m driving down a roadway,’ the therapist sets it up,” Rizzo says. If the memory happened around noon, the therapist sets the virtual clock accordingly. If the patient recalls the rumble of a Humvee, “Rrrrrp. Crank up the vehicle sound.”
Rizzo’s team tested an earlier version of the system by randomly assigning 162 military personnel to either a waiting list, 10 sessions of therapy that involved using the virtual Iraq/Afghanistan system or 10 sessions of traditional therapy. For traditional treatment, therapists coached patients through traumatic memories in their imaginations, and helped patients put themselves in everyday situations that they’d come to fear because of their trauma, such as crowded public places. Immediately after the study, both treatment groups showed substantial improvement in PTSD symptoms compared with those on the wait list, the researchers reported in November 2016 in the Journal of Consulting and Clinical Psychology.
“The real question is, if VR is as good as traditional therapies, which one should we do for which patients, and why?” says Greg Reger, a clinical psychologist at the University of Washington and VA Puget Sound Health Care System in Seattle.
By analyzing a subset of military personnel from the 2016 study, Reger and colleagues identified a few factors — like being younger and not taking antidepressants — that seemed to point to people who would fare better with VR. It makes sense that younger folks would be more responsive to tech-heavy treatment, but researchers have no idea why medication use would be relevant. Further investigations like Reger’s, reported in the June Depression and Anxiety, could help therapists decide when to pull out the headset.
Through the looking glass
To clinical psychologist Daniel Freeman of the University of Oxford, “the beauty of VR” is that it goes beyond rendering realistic experiences. “You can do stuff that you can’t do in real life.”
For instance, coaching a socially anxious patient through a conversation often involves redirecting that person’s attention away from themselves and toward their environment, he says. In VR, a therapist can direct a patient’s attention to particular aspects of the virtual world to help him or her forget their self-consciousness.
Gerard Jounghyun Kim, a computer scientist at Korea University in Seoul, and colleagues are testing a mix of real and fantastical elements to help people with panic disorder. In the researchers’ new VR program, a user can visit a potentially panic-inducing situation, like a parade or a crowded elevator. If a panic attack ensues, the user can hit an escape button and be transported to a peaceful beach. In that safe haven, patients get instructions to calm their breathing, while they hold a thumping device in their hand and see a virtual heart that pumps in time with their own.

This pilot trial, presented in 2017 in Gothenburg, Sweden, at the ACM Symposium on Virtual Reality Software and Technology, was much too small to show exactly how helpful this system might be for patients with panic disorder. Kim and colleagues are now doing a more comprehensive analysis with dozens of patients.
Face time
While Kim’s team is creating virtual versions of patients’ hearts, a group in Canada is rendering virtual bodies for the voices inside the minds of patients with schizophrenia.
Many people who take antipsychotic medication for schizophrenia continue hearing voices, says Alexandre Dumais, a psychiatrist at the University of Montreal. Traditionally, therapists advise patients to ignore these residual hallucinations, but recent research has shown that engaging the voices in conversation may actually help reduce patients’ sense of helplessness.
So Dumais’ team built a VR system in which a patient designs an avatar that embodies a bothersome hallucinatory voice. The therapist voices this avatar using patient-suggested sentences and gradually makes the avatar friendlier, encouraging the patient to get more comfortable and assertive in addressing the voice.
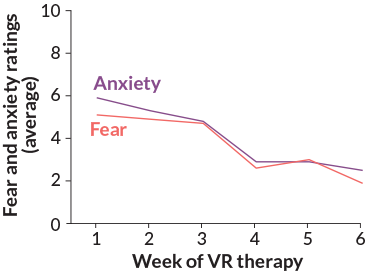
Dumais’ team tested this system, described in July in Schizophrenia Research, on 19 patients with schizophrenia. Four dropped out after the first session because they either didn’t like the program or found it too scary. The remaining 15 rated how scary they found each VR therapy session from 0 to 10, with 10 being the most distressing. Scores dropped over six weekly sessions. Moreover, at the end of treatment, the patients’ scores on a 0 to 20 scale measuring general hallucination-related distress dropped from an average of 16.1 to 10.9.
“We’re very much in the early days” of simulating impossible situations in VR for therapeutic purposes, Freeman says. But as VR becomes more pervasive, more researchers may have the opportunity to develop creative new treatments that exploit virtual unreality.
DIY therapy
Virtual avatars, good for filling simulated coffee shops, may also serve as therapists, transforming VR from a tool available only in a clinic to a new type of self-help. This may be especially useful for patients who are averse to visiting a therapist, such as people with social anxiety or agoraphobia, or for people living in remote areas without access to specialists.
The first fully automated virtual reality therapy, designed for fear of heights, was described in the Lancet Psychiatry in August (SN: 8/4/18, p. 15). In this program, an animated therapist guides a patient up a 10-story office complex. The user performs increasingly difficult tasks, from standing near a drop-off to going out on a platform over a central atrium. The virtual therapist periodically checks how the patient is feeling and offers encouragement. Freeman and colleagues tested this program on 100 patients: Forty nine were randomly assigned to two weeks of VR treatment; the other 51 got no treatment.
“I anticipated it was just going to be like a game,” one VR participant said, but the program “pushed the limits in terms of what I thought I would be able to achieve.”
On a scale measuring fear of heights from 16 to 80, the scores of people who used the VR program dropped, on average, about 25 points after treatment. The no-treatment group kept about the same scores as before. While results are encouraging, researchers don’t yet know how this program measures up to real-life therapy.
SUCH GREAT HEIGHTS In one fully automated VR therapy program, a virtual therapist helps users overcome their fear of heights by guiding them through a tall building with floors overlooking an atrium. Patients must complete challenges on each floor, including crossing a rope bridge. |
Another self-led treatment, this one to calm fear of spiders, has been tested against face-to-face therapy. The three-hour VR program involves various arachnids — a cartoonish, slipper-wearing spider to a realistic tarantula. The spiders approach the user while a virtual therapist offers instructions and encouragement.
“I’m not sure if anyone ripped the headset off, but a lot of people definitely started crying,” says Philip Lindner, a clinical psychologist at Stockholm University. One patient who was virtually sitting in a living room with a lot of spiders crawling around on the floor “physically put up her legs and sat like that for, like, 15 minutes.”
Researchers tested this system on 97 arachnophobia patients and described the results last November in San Diego at the Annual Association for Behavioral and Cognitive Therapies Convention. Half of the volunteers were randomly assigned to receive VR therapy and then encouraged to try approaching spiders in the real world. The other half completed a three-hour session of normal exposure therapy, where participants worked up from catching spiders in cups to holding a spider in each hand.
Before treatment, both sets of participants generally wouldn’t go near a spider in a clear container, Lindner says. After treatment, VR participants could stand next to or even put their hands inside the container, and real-world exposure patients could touch the spider. One year later, though, some VR patients could touch the spider too.
Lindner suspects that the VR experience reduced patients’ fears enough for them to try real-world exposure on their own, so they caught up with the normal exposure group.

Despite the early successes for specific phobias, it’s unclear whether therapist-free VR therapy for more complex disorders could be used at home.
In simulated social interactions, therapists carefully control virtual avatars’ responses to address each patient’s idiosyncratic anxieties. Computer-generated therapists aren’t yet so versatile that they can have conversations with patients that go in any direction, Bouchard says. He does believe, however, that virtual humans will eventually reach that level of sophistication. Even if virtual therapists are up to the job, many patients may not be driven enough to complete treatment on their own, Lindner says. “There was a lot of hype about [smartphone] mental health apps, and very few of them saw any kind of extensive real-world use.”
Motivation isn’t the only barrier to self-help. In some cases, self-led therapy may simply be too stressful. For patients using the personified-hallucinations program, “it’s really difficult to do at the beginning, because you’re hearing really bad things, like, ‘You’re an asshole, go kill yourself,’ ” Dumais says. “I don’t think a person can manage that alone.”
But developers shouldn’t discount potential stand-alone treatments before they’ve been tested, Reger says. These systems may make therapy, at least for some disorders, accessible to many patients who can’t or don’t want to see a human therapist. If automated treatments for complex disorders like PTSD were found safe and effective, he says, “I would certainly be a fan.”
This article appears in the November 10, 2018 issue of Science News with the headline, “Erasing Fear: Virtual reality therapy has real-life benefits for some disorders.”
Editor’s Note: This story was updated December 11, 2018, to correct a video credit. The grocery store video was produced by CleVR.net.