Stents Stumble
Enthusiasm wanes for drug-coated artery tubes
At a cardiology meeting in Stockholm 6 years ago, attendees witnessed what seemed to be the birth of a new era in treating heart disease. In the first large study of drug-coated stents—tiny mesh tubes that prop open clogged arteries—all the implanted arteries stayed open. The data were so stunning that after French researcher Marie-Claude Morice presented the study results, audience members stood and applauded.
“I remember it well,” says Robert Harrington of Duke University Medical Center in Durham, N.C. “You don’t see people get a standing ovation at a scientific meeting. There was this tremendous hope that we had finally beat it.”
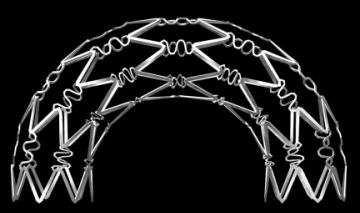
The “it” was restenosis, the renarrowing of arteries propped open by stents. Caused by tissue growing on the stent like moss invading a hollow tree trunk, restenosis is the main drawback of non-drug-coated, or bare-metal, stents. It leads to repeat procedures in about 30 percent of patients with those devices.
The dramatic data that Morice, of the Institut Cardiovasculaire Paris Sud, presented in Stockholm showed that 6 months after implantation of stents coated with drugs that inhibit tissue growth, an astonishing zero percent of arteries had reclosed. “We are probably witnessing a new revolution in the treatment of coronary disease,” Morice announced to the packed hall.
After the drug-coated stents gained regulatory approval in Europe in 2002 and in the United States in 2003, cardiologists eagerly adopted them. Soon, 90 percent or more of all implanted stents were of the drug-coated variety. Today, some 4 million to 6 million people worldwide carry them.
But now, interventional cardiologists are sitting on their hands.
A series of setbacks has thrown the field into turmoil. In 2004, researchers first reported seeing potentially deadly blood clots in patients who had undergone stent insertion a year or more earlier. Large studies later confirmed that finding. This April, another study showed that oral drug therapy may be just as good as stent implantation in treating mild artery blockage. Also in April, researchers reported that in patients with severe arterial disease, drug-coated stents offered no benefit over heart-bypass surgery.
A growing chorus of cardiologists and other observers now complains that hype outstripped evidence for drug-coated stents. They say that the devices were too often used on high-risk patients with severe coronary artery problems who should have undergone heart-bypass surgery instead.
The Food and Drug Administration stepped in last December, calling a special meeting to consider safety issues. The agency is now working with the makers of the two approved drug-coated stents to strengthen packaging language—the FDA’s equivalent of handing out a speeding ticket.
Says Mark Eisenberg, a cardiologist at the Jewish General Hospital in Montreal: “I think the interventional [cardiology] community is completely confused at this point.”
Delayed clots
In patients with coronary artery disease, the leading cause of death in the United States, fats and other detritus stick to the lining of the blood vessels supplying the heart. The disease first manifests as chest pain, but if the arterial plaques break free and block the vessel, a heart attack can follow.
Cardiologists often treat blockages that don’t critically limit blood flow with drugs that reduce cholesterol and prevent blood clots. In severe cases, they generally recommend bypass surgery to reroute the blood supply around the blocked vessels. In the 1990s, they began implanting bare-metal stents in arteries to keep them open.
After the restenosis problem became apparent, stent makers struck on a novel approach—coating the stents with drugs to prevent the tissue growth that causes restenosis. The two drug-coated stents on the market use cancer drugs—paclitaxel in one, sirolimus in the other—that kill fast-growing cells.
The first signs of trouble appeared in fall 2004, when a study in the Lancet reported that four patients had life-threatening blood clots 11 months or more after receiving drug-coated stents. The report worried cardiologists because while blood clots sometimes appear in the first few days after implanting a stent, late blood clots in patients with bare-metal stents were virtually unheard of.
“There were increasing numbers of case reports of this, and it was a new phenomenon,” says Eisenberg. Research teams began monitoring stent patients over the long term. “We identified that, yes, in fact, this is a real issue [that] affects just the drug-eluting stents” and not the bare-metal stents, Eisenberg says.
This year in the Feb. 24 Lancet, a European team reported that blood clots continue to occur in patients up to 3 years after insertion of drug-coated stents. The study followed 8,146 patients and found that about 0.6 percent per year suffered life-threatening blood clots.
While the percentage of problems reported is small, the sheer volume of people receiving the stents means that thousands of patients each year suffer blood clots that can lead to heart attacks and death.
Neal Kleiman, a cardiologist at the Methodist Hospital in Houston, says that he tries to keep the issue in perspective. “I think [concern] has been a little overblown. . ..I don’t think [blood clots are] the principle risk in these people’s lives.”
The reports of late blood clots ignited a debate over how long to maintain patients on aspirin and clopidogrel (Plavix), both of which prevent clotting. The FDA-approved packaging for the stents calls for 3 to 6 months of anticlotting drugs, but many cardiologists are now keeping patients on the drugs for 12 months or more.
After the December meeting, the FDA acknowledged an acute need for more data but issued a statement maintaining that “concerns about thrombosis do not outweigh the benefits” of drug-coated stents when the stents are used for “approved indications.”
And there’s the rub. The agency approved the stents for only a specific group of low-risk patients—those with one small blockage in one artery. But according to two studies in the May 9 Journal of the American Medical Association (JAMA), about half of patients who receive drug-coated stents do not fall in that category.
Stent who?
Off-label use is common in medicine. Makers of a drug or device seek FDA approval for a specific condition, but once approval is granted, physicians are free to use the therapy however they see fit.
For drug-coated stents, “there was off-label use like you’ve never seen,” says Michael J. Mack, director of the Cardiopulmonary Research Science and Technology Institute in Dallas. “I think this was mainly due to the marketing hype.”
As soon as the stents were approved, cardiologists ventured into unknown territory, implanting stents in patients with serious disease even though physicians had no information on the suitability of the devices for those conditions. They stuck two stents end to end to treat long blockages; they stented V-shaped blockages at the juncture of two arteries; they restented arteries that had collapsed after earlier procedures; and they stented the large left-main artery, which supplies 75 percent of the heart’s blood. They even triple-stented patients with three blocked vessels, a deadly serious condition formerly treated only by surgery.
“What surgeons have heartburn about in all this is that the increase in off-label use came at the expense of coronary-bypass surgery,” says Mack, a surgeon. “It’s all gone to drug-eluting stents without good evidence.”
Not surprisingly, patients who receive stents for the more complicated off-label conditions fare worse than do their lower-risk peers, according to the two JAMA reports. The first report described a study of 6,993 patients. After a year, 4.3 percent of those receiving stents for the serious off-label conditions had died, whereas 2.6 percent of the on-label group had died. In the off-label group, the rate of blood clots at 1 year was twice as high, and about twice as many patients returned to the hospital for an additional stent or surgery compared with the results in patients with on-label conditions.
Despite this, report coauthor Charles Davidson, a cardiologist at the Northwestern University Feinberg School of Medicine in Chicago, says that “absolute rates of adverse events are low” and “the safety profile appears excellent” for all patients receiving drug-coated stents.
The second JAMA study, though, came to a more troubling conclusion. Drawing from a different database of 3,323 patients, the study found that within a year, 18 percent of patients with the most serious, off-label diseases had died, had a heart attack, or needed an additional stent or surgery. The figure for patients with on-label conditions was about 9 percent.
Kleiman, who coauthored the report, says, “Something is going on, and it may just be that these [off-label] folks are sicker. It may be that the drug-eluting stents carry more of a risk with them. Or it may be both.”
Who pays?
As for why the second study reported a higher rate of bad outcomes than the first, Duke University’s Harrington invokes sponsor bias. The first study, in which the authors conclude that the overall rate of negative events was low, was sponsored by Cordis, the division of Johnson & Johnson that makes drug-coated stents. Millennium Pharmaceuticals and Schering Plough Inc., makers of anticlotting drugs, paid for the second study, which found much higher rates of poor outcomes.
“If you’re an [anticlotting-drug] manufacturer, it’s in your best interest to demonstrate that the risk of these procedures is high, because you have a therapy that might lower that risk,” Harrington says. “If you’re a drug-eluting-stent manufacturer, it’s in your best interest to show the procedures are very safe.”
Whatever the true rate of poor outcomes in the on- and off-label groups, the use of drug-coated stents is down sharply this spring. Harrington says that at Duke, about 50 percent of implanted stents are now drug coated, down from about 90 percent last fall. Information from 400 hospitals across the United States shows that, in March, drug coated stents accounted for 73 percent of all stents implanted, down from about 90 percent last fall. “I think it’s almost exclusively the late [blood-clot] issue,” says Harrington.
But other stent skeptics cite an additional factor. A study in the April 12 New England Journal of Medicine (NEJM) showed that patients with mild arterial disease fared just as well without stents as they did with them, as long as they took standard medication, including blood thinners and beta blockers. After almost 5 years, about 19 percent had died among patients who got stents and medication and among those who got medication alone.
Judith Hochman of the New York University School of Medicine says in an accompanying NEJM editorial that the study should be a clear signal to doctors to reduce stent implantation in patients whose arterial plaques aren’t immediately life threatening. About 85 percent of stents are implanted in such patients.
Also in April, researchers at an American Heart Association meeting in Chicago reported that, in high-risk patients, drug-eluting stents offered no advantage over heart-bypass surgery. The study found similar rates of severe complications, such as heart attacks, in the first month after treatment. Death rates after 3 years were similar. Study leader James Wilson of the Texas Heart Institute in Houston says that the findings from the study, the first head-to-head comparison of bypass surgery and drug-coated stents, were “a bit of a surprise.” Cardiologists had expected fewer complications from stents.
Adding to the glum news for cardiologists, this spring Johnson & Johnson halted a clinical trial of its next-generation drug-coated stent. Early data showed that the new stent didn’t help patients any more than existing devices did, says the company.
However, a glimmer of hope appeared in the June 2 Lancet, where researchers report favorable early results for a new, biodegradable stent (SN: 6/9/07, p. 356). This stent disappears after a few months, and, though results are preliminary, cardiologists hope that the threat of late blood clots will vanish with it.
Every expert interviewed for this article expects the FDA to tighten monitoring of stents and to ask manufacturers of new devices to provide more data on a wider range of patients, such as those with more complex disease. Stent manufacturers have vowed to keep a closer eye on the safety of their products.
Observers predict a continuing decline in the use of drug-coated stents. Says Eisenberg: “This is one of those situations where we thought there was no downside. But now that there is a serious downside, even if the risk is tiny, most of us are very risk averse. So I need to be convinced now by hard data that a drug-coated stent is the right way to go.”