Sleep Gone Awry
Researchers inch closer to causes, cures for insomnia, narcolepsy
- More than 2 years ago
If Ben Franklin had been able to live by his own advice, he might have been even healthier, wealthier and wiser. But he was a notorious insomniac, rumored to have been such a poor sleeper that he required two beds so he could always crawl into one with cool sheets when he couldn’t sleep. Getting a good night’s sleep turned out to be more difficult than taming lightning, heating houses or designing bifocal specs.
Today millions of people afflicted by sleep disorders know how Franklin felt. Some people can’t fall asleep even when they’re exhausted. Yet other people fall asleep when they should be wide awake. Although sleep disorders take many different forms, they do have one thing in common: The more researchers learn, the more they have left to figure out. Sleep problems present a constellation of symptoms, trigger overlapping diagnoses and divulge no clear causes.
“We always feel like we’re one step away from getting all of the answers,” says Adi Aran of Stanford University, “but I really believe that in the next decade we will understand much more about sleep disorders.”
Already, some recent advances have brought scientists closer to discerning the ultimate causes of such disorders, even suggesting possible treatments. Masashi Yanagisawa of the University of Texas Southwestern Medical Center at Dallas believes researchers are poised to “crack open the black box of sleep regulation.”
Glimpses into that black box suggest that insomnia stems from overactive body systems that conspire to overtake a perfectly functional sleep system. Two reports find that one measure of arousal, blood pressure, is elevated in people with insomnia even while they are asleep.
Other glimpses come from studies of narcolepsy. Scientists have known for almost a decade that narcolepsy is caused by a dearth of a brain communication chemical called orexin. But researchers are still struggling to explain why the neurons that produce orexin are lost in the brains of people with narcolepsy. New evidence implicates a malfunction of the immune system as a likely culprit.
Understanding what goes wrong in sleep disorders such as narcolepsy and insomnia may lead to more targeted treatments. Instead of flooding an insomniac’s brain with a general depressant, clinicians may one day specifically target particular overactive brain regions. Rather than giving people with narcolepsy stimulants that rev up the entire body, preventive measures may halt neuron death before narcolepsy sets in. More generally, understanding these disorders may help researchers create a more complete picture of normal sleep and normal wakefulness, and how bodies and brains transition between the two.

Sleepless nights
For some people, the Franklinesque advice to go to bed early is impossible. Trouble falling asleep or staying asleep (or waking up still tired) is loosely defined as insomnia. It’s a big problem: The National Center on Sleep Disorders Research reports that 30 to 40 percent of Americans say they suffer insomnia symptoms at least once over the course of a year.
“Almost everybody has insomnia at some point in their life,” says Michael Bonnet of Wright State University’s Boonshoft School of Medicine in Dayton, Ohio.
Sleeplessness may be brought on by traumatic events such as a death in the family, an illness such as cancer or anything else distressing, causing a person to lie awake at night with a racing mind. For a subset of people, though, insomnia has no prompting signal — a condition called primary insomnia.
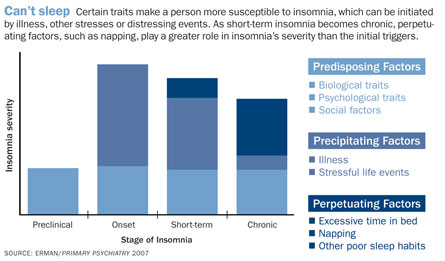
Regardless of the trigger (or lack thereof), temporary insomnia has a nasty way of becoming a habit. Poor sleep habits can become ingrained. When trouble sleeping persists for three or four nights a week over several months, insomnia is considered chronic.
It may turn out that untangling the prompting signals of insomnia, as many sleep researchers attempt, is a fool’s errand, says Michael Perlis, director of the University of Pennsylvania’s Behavioral Sleep Medicine Program in Philadelphia. “The whole zeitgeist has changed,” he says. Most sleep researchers now agree that “once insomnia goes chronic, it stays that way,” regardless of the prompting signal, Perlis says. So rather than focusing on the immediate trigger for insomnia, many scientists are trying to figure out why it becomes chronic and how to prevent that from happening.
A growing body of evidence supports a hyperarousal explanation of chronic insomnia, in which the sleep centers in the brain are overwhelmed by amped-up “awake” signals.
For instance, people with primary insomnia have higher hormone secretions, higher body metabolism, heightened activity in certain brain regions and elevated heart rates, studies show. Even body temperatures may be raised in people with primary insomnia. This heightened activation is present in the day and remains through the night.
After a traumatic event or a fright, the body and brain are in an aroused state. Heartbeat increases, blood flows faster and stress hormones flood the body, putting the muscles and the brain on high alert, ready to quickly deal with whatever comes next. A meeker version of this excited state might be what keeps people with insomnia awake, Perlis says. People with insomnia don’t constantly have the extreme palpitations that come from an encounter with Freddy Krueger, he says. “We’re hardly talking about panting and heart thumping.”
But the heightened alertness is just enough to interfere with sleeping, making insomnia more of a disorder of wakefulness than of sleep. “Patients with insomnia in general could have a fairly decent sleep system,” Bonnet says. “And that’s kind of hard for a sleep researcher like myself to say.”
Two reports make the case that people with insomnia are hyperaroused, Bonnet says. A case-controlled study conducted in a Canadian sleep lab found that 13 patients with primary insomnia had higher systolic blood pressure than people in a comparison group. What’s more, those people with insomnia failed to show the characteristic dip in systolic blood pressure when day turns to night. Heightened brain activity at night correlated with higher blood pressure, researchers led by Paola Lanfranchi at the H´pital du Sacré-Coeur de Montréal reported June 1 in Sleep.
A larger study of 1,741 people from central Pennsylvania found that people with chronic insomnia and short sleep duration (as measured in a sleep lab) were more likely to have high blood pressure. Cardiovascular diseases including strokes and heart attacks may go hand in hand with chronic insomnia, Alexandros Vgontzas of Pennsylvania State University College of Medicine in Hershey and colleagues suggest in their paper in the April 1 Sleep.
Other reports show that regions of the brain remain unduly active in people with insomnia, including the hypothalamus, a brain center important for sleep and arousal. In the not-too-distant future, Bonnet says, scientists may identify the precise brain regions where activity is too high at night, and the regions that tell the body to rev up. “Obviously once you’ve found specific brain areas where you have activation, you can find ways to direct drugs to those areas,” he says.
Treating a disorder before it is fully understood is hard, but researchers are developing some new therapies that seem to work. Several reports over the last few years have explored a treatment called cognitive behavioral therapy for insomnia, or CBTi. The method works by training people to change behaviors that interfere with sleep. Participants are instructed to avoid naps, get out of bed if they’re not sleeping and stop stressing over lost z’s, all steps that can boost sleep. Continued practice of CBTi may reprogram the parts of the brain that control the sleep-wake cycles. “Even though we know not what we deal with, CBTi is highly effective,” says Perlis, a strong proponent of such behavioral interventions.
While peeking into the black box of insomnia reveals an array of overactive body and brain offenders, the black box of another sleep disorder — sleep-inducing narcolepsy — holds just one culprit: a small group of specialized neurons that make a chemical with two names.
Narcobiochemistry
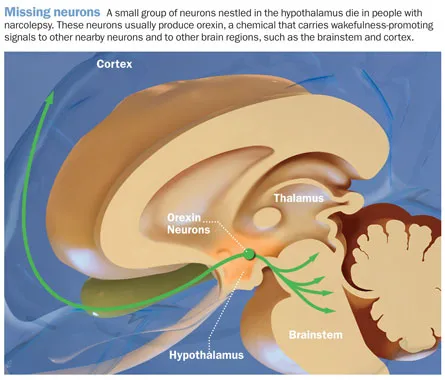
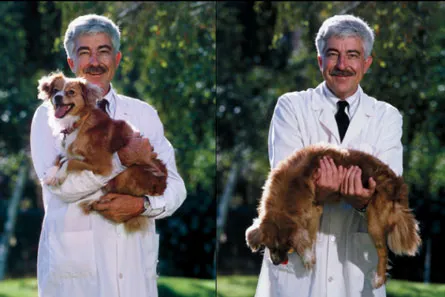
About a decade ago, experiments by Yanagisawa with mice and by other researchers with dogs found that narcolepsy is almost certainly caused by the absence of a single chemical messenger in the brain. This chemical, called orexin by some scientists and hypocretin by others, is produced by a small pocket of neurons in the hypothalamus. “Narcolepsy is very special in the whole variety of sleep disorders,” Yanagisawa says. “So far, narcolepsy is the only sleep disorder that has been reduced to the biochemical level.”
People lacking orexin-producing neurons fall asleep uncontrollably. In extreme forms of narcolepsy, this happens every one to three hours. Narcoleptic attacks can also be accompanied by a loss of muscle tone, called cataplexy. Severe cataplexy can leave the entire body as limp as a rag doll.
Examining brains from people who had narcolepsy, researchers found that the neurons in the hypothalamus that secrete orexin are almost completely absent. Narcoleptic brains had an 85 to 95 percent reduction in orexin neurons, Jerome Siegel, of the University of California, Los Angeles and his colleagues found. Since that study, published in 2000, scientists have been intent on figuring out how these neurons die, in order to find a way to prevent narcolepsy by helping the cells survive.
One possible suspect is the immune system, which ordinarily protects the body from harmful outside threats. Genetic studies in the 1990s provided a strong hint for the immune system’s role: About 90 percent of people with narcolepsy have the immune gene variant HLA-DQB1*0602, whereas only about 25 percent of the normal population carries that variant. HLA genes encode proteins that sit on the outside of cells and help the immune system recognize the body’s own cells. In people with this variant, the reasoning goes, self-recognition may be more likely to go awry, causing the immune system to attack this small, important population of neurons in the hypothalamus.
Recent work from Emmanuel Mignot, a sleep researcher at Stanford University, and his colleagues uncovered another immune system link. A study of over 4,000 people found that those with narcolepsy were more likely than others to have a certain DNA letter in part of a gene called the T-cell receptor alpha locus. This gene codes for a protein that recognizes the HLA pattern on the outside of cells. Erroneous readings of the HLA pattern might cause an immune cell to mount an attack on the body’s own orexin-producing neurons, the authors hypothesize in a report published in Nature Genetics in June.
Another recent study found that certain bacterial infections might spur the destruction of these neurons. In some diseases, streptococcus infection has been shown to trigger autoimmune attacks. It may signal the body to mistakenly kill orexin neurons too. “It makes sense that these cells die due to some kind of inflammation,” says Aran, who collaborated with Mignot on the research, which appeared August 1 in Sleep.
In the study, people with newly diagnosed narcolepsy had higher blood levels of strep antibodies than did controls, suggesting the patients’ immune systems were geared up to fight off an infection. What’s more, this antibody response lingered for up to three years in people with narcolepsy, whereas the antibody levels go down in just months in most healthy people. “We believe that strep infection might be one of the triggers for narcolepsy,” says Aran. “We don’t know exactly how, but we believe streptococcus does something.”
Identifying the autoimmune response trigger (or triggers) would still not answer the greater mystery, though. Scientists remain baffled by how the immune system conducts such a targeted kill-off of orexin neurons. Almost all of the orexin neurons are destroyed, while other kinds of neurons — even those nearby — remain untouched. Presumably, orexin neurons have some identifying mark that the immune system specifically detects, but so far, that mark is a mystery. “Despite over 15 years of research, no one knows,” says Aran.
Current treatments for narcolepsy, while somewhat effective, address only the symptoms, not the underlying loss of neurons. In most cases, once the symptoms show up, the neurons are already gone, says Aran. “If we know the exact pathogen, it might prevent some of the cases,” he says. If strep is verified as a trigger, preventing such infections in people — especially those with the particular HLA variant that makes them susceptible — might thwart narcolepsy.
Uncovering the root causes of sleep disorders will undoubtedly lead to better therapies, and maybe even preventions. More than that, though, scientists may have a better chance of learning what happens when sleep goes right — a question that remains largely unanswered — by understanding how sleep goes wrong. “One of the very satisfying things,” Siegel says, “is that it gives you insight into how sleep and wake are controlled.”
|
Sleep gone bad Restless legs syndrome |