More than a Kick
On its own, nicotine might promote tumors and wrinkles
- More than 2 years ago
Nicotine shifts the body into high gear. Whether from a puff on a cigarette or a patch stuck to the skin, the drug enters the bloodstream and bathes the internal organs. But scientists generally attribute nicotine’s power solely to the activity it sparks in the brain. That stimulation makes smokers feel good, even euphoric. It’s also what makes them crave more. Physicians, however, generally finger

tobacco’s thousands of other chemical constituents, including known carcinogens–not nicotine–for cigarettes’ nastiest side effects. Each year, tobacco accounts for 400,000 deaths among 48 million smokers in the United States alone.
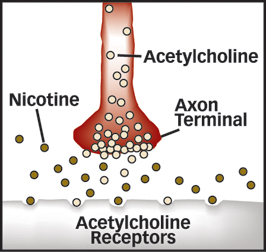
Beyond its addictive appeal, nicotine itself might have devastating consequences throughout the body, some scientists now say. Acetylcholine–the natural nerve-signal carrier that nicotine mimics–is a jack-of-all-trades. The chemical acts on many cells, including those in the lungs and skin. Therefore, nicotine may goad many tissues into hyperactivity–a possibility that raises scientists’ suspicions about its role in disease.
“It’s an eye opener. Nicotine isn’t just a drug that stimulates neurons. It does the exact same thing to cells outside of the nervous system,” says dermatologist Sergei A. Grando of the University of California, Davis, who studies nicotine’s effects on skin.
A handful of recent studies has suggested a link between nicotine and ailments ranging from sudden infant death syndrome (SN: 9/14/02, p. 163: Available to subscribers at Smoking Gun? Mouse tests link nicotine to crib death) to cancer. Scientists have found that the stimulant spurs the formation of blood vessels that could feed tumors and promote plaque buildup in arteries (SN: 7/7/01, p. 6: Nicotine spurs vessel growth, maybe cancer). The body may also convert nicotine into the chemical precursors of the carcinogen that scientists call NNK (SN: 10/28/00, p. 278: Nicotine metabolism may spawn carcinogen).
The latest experimental work strengthens the connection between nicotine and disease and highlights additional ways that the chemical might promote tumors, age skin, and stall wound healing. Researchers say the drug may also literally cook proteins in the blood.
Death can be good
Nicotine probably doesn’t cause cancer, but new research suggests it might keep cancer cells alive. And it apparently does so in two different ways.
First, the drug prevents a cellular form of suicide, called apoptosis, that normally eliminates nascent cancer and other damaged cells, says clinical oncologist Phillip A. Dennis of the National Cancer Institute in Bethesda, Md.
In many cancers–including those of the breast, ovaries, prostate, and brain–a protein that normally keeps apoptosis under control gets stuck in its active form and thus shuts down the suicide sequence. More recently, Dennis’ team discovered that the same molecule, called either Akt or protein kinase B, jams in the on-position in most lung cancer cells. The finding led the team to wonder whether constituents of tobacco activate Akt in the lung.
To find out, they tested the effect of nicotine and its derivative NNK on normal lung cells in lab dishes. Nicotine activated Akt at concentrations comparable to those that have been measured in smokers’ blood, and the cell-suicide rate fell by 60 percent, the team reports in the January Journal of Clinical Investigation. It took more stress–ultraviolet radiation exposure, for example–to kill nicotine-activated cells than normal cells required, Dennis says.
Nicotine-treated cells acted abnormal in other ways, too. In lab dishes, lung cells usually stop growing when they become crowded, Dennis explains. “When treated with nicotine, lung cells kept growing to the point of coming right out of the plastic,” he says.
NNK also enhanced cell survival by stimulating Akt. Therefore, NNK might exacerbate nicotine’s cancer-promoting ability, Dennis suggests.
Nicotine’s boost to cell survival could be important to other cancers associated with tobacco, including those of the head, neck, kidney, and bladder, he says.
Nicotine has a second talent for enhancing tumor growth, two lines of research suggest. The drug makes tumor-nurturing blood vessels sprout. Tumors can only grow to a certain point before they must be fed, says John P. Cooke of Stanford University. “They don’t continue to grow and become malignant unless they can call blood vessels into themselves,” he says.
Cooke’s team has found that nicotine increases the speed at which human blood vessel cells grow in lab dishes. What’s more, lung-tumor cells in mice given nicotine-laced water expanded faster than those in mice not given the drug (SN: 7/7/01, p. 6: Nicotine spurs vessel growth, maybe cancer).
Nicotine may encourage blood vessel formation by stimulating the production of vascular endothelial growth factor, or VEGF, a second team of researchers has found. Vascular-system researcher Brian S. Conklin, now at Baylor College of Medicine in Houston, and his colleagues knew that VEGF shows up in the majority of cancerous tumors. It’s also a player in plaque formation along blood vessel walls.
Because vascular disease and cancer are both linked to smoking, Conklin and his colleagues wondered whether nicotine might ramp up blood concentrations of the growth factor.
The team tested the effects of nicotine and cotinine–the primary product of nicotine breakdown in the liver–on blood concentrations of VEGF in a pig artery. Both compounds hiked concentrations of the growth factor, the researchers reported in the February 2002 American Journal of Pathology.
Full speed ahead
Just as nicotine sparks activity in nerve and tumor cells, it speeds up normal cellular activity in the skin. For example, some cells exposed to nicotine might go through the same life stages in 10 days that would normally take 10 weeks, says dermatologist Grando.
Such hyperactivity occurs in cells called dermal fibroblasts that control the skin’s texture by regulating the production of support proteins including collagen and elastin. When skin gets wounded, these fibroblasts send out proteins that clean the site. The cleanup crew acts like “biological scissors,” Grando says, clearing the way for healing to begin.
In the February Laboratory Investigation, the team reports that nicotine sends fibroblasts into inappropriate activity. In the laboratory, the researchers exposed human fibroblast cells to the drug. Enzymes normally unleashed to clean wound sites were deployed in the absence of injury. Those proteins then chewed up the scaffolding that keeps skin flexible and strong. That effect would leave skin sagging and wrinkled, Grando explains.
On the other hand, in regular users of tobacco, another mechanism of skin healing slows down as a result of nicotine’s ability to speed cells up. Normally at a cut, skin cells called keratinocytes crawl out from the edge of a wound and cover the broken surface. Acetylcholine sets those cellular healers in motion. That led Grando and his colleagues to ask whether nicotine interferes with keratinocyte migration.
The researchers grew human skin cells in lab dishes and treated some cells with growth factors and others with growth factors in combination with nicotine.
Nicotine-treated cells started to move as if on a healing mission but stopped short of the distance that cells not given nicotine traveled, the team reported 2 years ago. The span traveled by keratinocytes declined further as more nicotine was added to the lab dishes.
The fast-paced lifestyle that nicotine induces in cells might explain why, Grando says. Nicotine cuts skin cells’ active life short, leaving them with too little time to seal a wound before they conk out, he hypothesizes.
Now we’re cooking
Nicotine’s widespread effects result primarily from its imitating the natural stimulant acetylcholine. But a new study suggests that a derivative of the drug might also interact with the blood to literally fry proteins.
While poring over the chemical structure of nornicotine–a minor metabolite of nicotine–chemist Kim D. Janda of Scripps Research Institute in La Jolla, Calif., recognized that the compound has the potential to mangle proteins. The metabolite could spur the same chemical transformation that occurs when potatoes are fried, he suspected, a reaction familiar to food scientists as the browning effect. A similar reaction can occur without the high temperatures, Janda explains. Proteins altered in this way have been implicated in diabetes, cancer, and normal aging.
In the laboratory, Janda and his colleagues added nornicotine to solutions of blood proteins. Nornicotine attached to the proteins, so that at the molecular level, the product looked like “Christmas trees with nornicotine lightbulbs on them,” Janda says. When food browns, similar structures result.
In separate experiments on whole blood from smokers and nonsmokers, the team found that smokers’ blood contains more such nornicotine-altered proteins than nonsmokers’ blood does. The researchers reported their findings in the Nov. 12, 2002 Proceedings of the National Academy of Sciences.
“It’s pretty shocking,” says Janda. “Nornicotine can be involved in a chemical reaction no one had thought about.” The team is now conducting studies to find out how common the nornicotine-blood reaction is in animals and people.
For people trying to kick the cigarette habit, gums, patches, lollipops, and lip balms that contain nicotine are often useful. High-dose nicotine replacements can deliver the stimulant at concentrations comparable to those in cigarettes while giving a person a more constant blood-nicotine concentration than smoking does and avoiding many of cigarettes’ harmful components.
“It’s still most important that people stop smoking–if they need [nicotine-replacement therapy] to do that, fine,” says oncologist Dennis. “But nicotine itself might be harmful in the long term,” he adds.
Some people use quitting aids for longer than the recommended few months. Ann N. Dapice, an educator at the addiction treatment center T. K. Wolf in Tulsa, Okla., says she’s worked with people who have used nicotine patches and gums for years.
Although scientists don’t know all of nicotine’s long-term effects in people, emerging evidence makes a “whole new case” for the drug’s potential to cause problems outside the nervous system, says oncologist John D. Minna of the University of Texas Southwestern Medical Center in Dallas.
And once scientists look closer, he adds, they might find disease connections to nicotine that haven’t been considered yet.
Not All Bad
A once-good-for-nothing drug improves its reputation
The properties that make nicotine a health hazard might also make it a useful therapy for more than smoking cessation. “Nicotine is a drug–not a poison or carcinogen–but a drug,” says Sergei A. Grando of the University of California, Davis. “Nicotine is often a bad guy,” he adds, “but it can also be a good guy.”
For one, nicotine can help alleviate the mind-numbing symptoms of Alzheimer’s disease. Alzheimer’s patients lack the normal number of one type of receptor that binds acetylcholine in the brain, making them less responsive to that nerve signal. The deficit leads to learning and memory problems, says neurobiologist Alfred Maelicke at Johannes-Gutenberg University in Mainz, Germany.
A similar shortfall plagues people with schizophrenia and epilepsy, among other disorders, he adds.
In such cases, intermittent nicotine boosts to the brain can help, Maelicke says. Nicotine patches may also fight depression (SN: 5/11/02, p. 302: Available to subscribers at Could nicotine patch fight depression?). And there’s more good news. Although regular nicotine use can delay wound healing, a new study finds that the stimulant speeds healing in mice with diabetes–a disease that normally impairs wound healing.
Prompted by his earlier discovery that nicotine spurs blood vessel growth, John P. Cooke of Stanford University wondered whether the drug might help close wounds. His team injured diabetic and nondiabetic mice and then applied a solution containing nicotine to some of the animals in each group.
After 5 days, diabetic mice receiving the nicotine treatment had healed substantially more than diabetic mice not getting the drug had, the team reported in the July 2002 American Journal of Pathology. Nondiabetic mice didn’t benefit from the treatment with nicotine.
That result makes sense to Grando. “Like any drug, the dose is important,” he explains. “At low doses, nicotine can favor faster wound healing, while in larger doses it has the opposite effect.”
The challenge in all nicotine’s possible uses is to identify people for whom the drug’s benefits outweigh its risks and to develop targeted delivery methods, says Phillip A. Dennis of the National Cancer Institute in Bethesda, Md.
****************
If you have a comment on this article that you would like considered for publication in Science News, please send it to editors@sciencenews.org.







