Lead’s damage can last a lifetime, or longer
Tainted water for kids in Flint could mean problems in adulthood

TOXIC WATER A mom in Flint, Mich., uses bottled water to bathe her three-week-old baby. Scientists have linked high levels of lead in the tap water there to elevated blood lead levels in children.
Todd McInturf/The Detroit News via AP
The people of Flint, Mich., are drinking bottled water now, if they can get it. Volunteers deliver it door-to-door and to local fire stations.
The goal is to keep the city’s residents from ingesting so much lead. Success – or lack thereof – could have consequences not just now, but for generations to come.
Late last year, scientists raised alarms over a link between the city’s lead-tainted water and the growing number of children with high lead levels in their blood. It’s a serious problem. Lead is toxic to the brain, something scientists have long known.
“Lead is probably the most well-known neurotoxin to man,” says Mona Hanna-Attisha, the pediatrician who first connected lead in Flint’s water to lead exposure in kids. And as scientists are beginning to find out, the damage that lead inflicts on children may be long-lasting. In addition to harming kids during youth, lead could contribute to disorders that develop later in life, such as Alzheimer’s disease or schizophrenia. Lead’s reach could extend even further, too — beyond those who drank the contaminated water to their children and grandchildren.
Flint’s kids “will have to be followed throughout their whole life, and maybe into the next generation or two,” says Douglas Ruden, a neural toxicologist at Wayne State University in Detroit.
A few months of drinking clean water will help bring the kids’ lead levels back down, he says. “But the damage is done.” And it’s permanent.
A history of lead
In the United States, lead is everywhere. Decades of burning leaded gasoline spewed lead into the air, and the element settled in the upper layer of soil, clinging to particles of dirt.
“Lead never goes away,” says David Bellinger, an environmental epidemiologist at Boston Children’s Hospital. “It doesn’t degrade. It just stays where it is.”
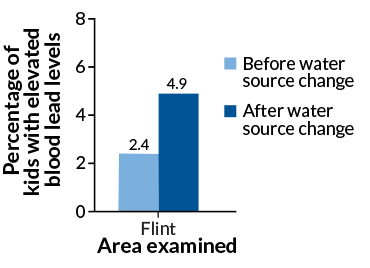
Indoors, old lead-based paint still flakes from houses, and in many U.S. cities, lead remains in old water pipes. In April 2014, a switch in Flint’s water source (from Lake Huron to the corrosive water of the Flint River) dissolved lead in the city’s pipes, letting the toxic metal seep into tap water. After the switch, the number of kids with elevated blood lead levels doubled; in some neighborhoods, it tripled, Hanna-Attisha, of Hurley Medical Center in Flint, reported February in the American Journal of Public Health.
Now, Hanna-Attisha is working with Ruden to examine lead levels in blood from babies born during the water crisis. The known spike in high lead levels “grossly underestimates the risk,” Hanna-Attisha says. It didn’t include newborns whose mothers had been drinking the contaminated water.
Flint’s crisis garnered national attention, in part because lead exposures in the United States have become less common over the past few decades.
“It’s actually a great public health success,” Bellinger says.
Since the United States banned lead in paint in 1978 and gasoline in 1996, the amount of lead in children’s blood has fallen hard and fast: from around 16 micrograms per deciliter of blood on average in the late 1970s to just over 1 mcg/dl in 2010. Today, 5 mcg/dl is the benchmark for high blood lead levels, according to the U.S. Centers for Disease Control and Prevention.
Most cases of lead exposure in children come from eating lead particles or paint.
Children playing outside or on the floor can end up licking lead dust that’s stuck to their hands or toys — it tastes sweet. From the mouth, lead travels to the gut, into the bloodstream, and on to the brain and other organs. Then lead moves into the bones, where it can hide out for decades.
Scientists have linked chronic lead exposure to lowered IQ, shortened attention spans, antisocial behavior and having less gray matter — the nerve cell bodies that makes up much of the brain.
“We know now that no amount of lead is good for children,” says neurotoxicologist Tomas Guilarte of Florida International University in Miami and Columbia University.
He and others have spent years puzzling out what lead does to the brain. It’s a grim picture. Chronic exposure can kill nerve cells, and make it hard for new ones to survive and talk to each other. The mark lead leaves on the brain might even show up when people age.
“I think in the next 15 to 20 years,” Guilarte says, “if people look closely, they’ll find that many of these lead-exposed children are going to have mental issues.”
Adult problems
In recent years, scientists have linked lead exposure to diseases that strike in adulthood, such as Alzheimer’s, Parkinson’s and schizophrenia.
Some evidence comes from animal studies. In 2015, Guilarte and colleagues chronically exposed young rats to lead and then dissected their brains. The rats showed signs of schizophrenia, the researchers reported in Translational Psychiatry. They had lost PVGI neurons, brain cells essential for attention and memory. And the rats had gained dopamine receptors, proteins that help brain cells receive chemical messages.
At the molecular level, one way lead might do its dirty work is by masquerading as zinc. One of zinc’s jobs is to anchor floppy sections of protein together, forming a shape that plugs into DNA. This lets proteins flip genes on and off like a light switch. When lead takes the place of zinc, the protein switch might not work the same way, says Rachel Austin, a bioinorganic chemist at Barnard College in New York City.
Scientists know that several of these switches go out of whack in schizophrenia, Alzheimer’s and Parkinson’s. Lead could bear some of the blame, Austin and Jacqueline Ordemann of Bates College in Lewiston, Maine proposed January 8 in Metallomics. “It’s certainly chemically possible,” Austin says.
Lead exposure during youth also seems to leave chemical fingerprints on future generations. Last September, Ruden and colleagues examined blood collected from 35 Michigan mothers and babies at birth. The newborns’ DNA carried an atypical set of chemical tags, or methyl groups, the researchers reported in Scientific Reports. Some of their mothers had high blood lead levels when they were born, which means that their mothers had been exposed to lead. So if grandma had lead in her blood, her grandkids will show it, the researchers concluded.
If DNA is the hardware of the cell, says Ruden, then the chemical tags are the software that tells cells what to do. Lead seems to rewrite cells’ software — for generations, he says. “We don’t know if that’s good, bad or indifferent,” he says. “But it’s more than likely not good.”
Search for treatments
Massive public health campaigns have tried to scrub lead from the environment, but there’s still no cure for lead poisoning. Some treatments, called chelation therapies, can draw lead from the body, but they don’t seem to help the brain. And dietary supplements, like iron or calcium or zinc, could potentially keep lead from entering into the blood, but “the evidence is not that great,” Bellinger says.
Still, Hanna-Attisha says the situation in Flint isn’t hopeless. Thousands of kids drank contaminated water, “but it doesn’t mean every kid is going to have every problem,” she says. And stimulating children’s learning might be one way to lessen lead’s damaging effects.
A 2013 study found a link between the home environments of lead-exposed first graders and their thinking ability and behavior. Lead seemed to have less of an effect on kids whose mothers helped out with schoolwork and extracurricular activities, Katarzyna Kordas and colleagues reported in NeuroToxicology.
“It’s certainly very suggestive, but we’re not claiming causality,” cautions Kordas, an environmental epidemiologist at the State University of New York at Buffalo.
Ultimately, preventing exposure to lead in the first place is key, says Hanna-Attisha. “You don’t mess around with lead,” she says. “It can change a child’s whole life trajectory.”
Editor’s note: This story was updated March 7, 2016, to include an additional affiliation for Tomas Guilarte.