Hallucinated voices’ attitudes vary with culture
Schizophrenia symptom turns positive in non-Western nations
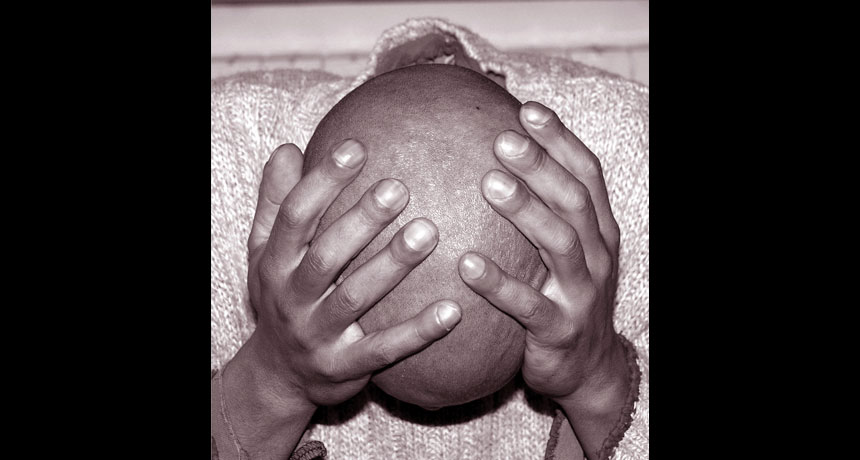
MISGUIDED BY VOICES Many people with schizophrenia report hearing voices, but these hallucinations are experienced as largely negative in the United States and as mainly positive in India and Ghana, a new study suggests.
t-lorien/iStockphoto
People with schizophrenia may hear either hostile voices goading them to jump off a bridge or a mother’s soothing words of advice, depending on the cultures in which they live, a new study suggests.
In the United States, schizophrenia’s symptoms include hallucinations of disembodied voices that hurl insults and make violent commands, says an international team led by Stanford University anthropologist Tanya Luhrmann. But in India and Ghana, schizophrenia patients often report positive relationships with hallucinated voices that they recognize as those of family members or God. The findings will be published in the January 2015 British Journal of Psychiatry.
“Learned cultural expectations about the nature of mind and self may encourage Americans with schizophrenia to pay more attention to negative, hostile voices,” Luhrmann says.
Much evidence shows that Westerners think of the mind as a fortress guarding private thoughts and of schizophrenia as a broken brain. Americans with schizophrenia in the new study — who often referred to hallucinated voices as unreal and as symptoms of a brain disease — homed in on the strangest, most antagonistic voices in their minds, Luhrmann suspects.
Indians and Africans in the study spoke little of their psychiatric diagnosis. Their social worlds emphasize relationships over individuality and the possibility of supernatural contacts with spirits. Many patients in both nations regarded most hallucinated voices as familiar people who couldn’t be controlled but who were sensible and likable.
Hearing voices, an experience reported by some mentally healthy people as well as those with schizophrenia (SN: 4/7/12, p. 22), “may be a partially learned and malleable skill,” says medical anthropologist Kim Hopper of Columbia University.
Luhrmann, working with two psychiatrists in India and one psychiatrist in Ghana, recruited 20 people in each country receiving hospital or outpatient treatment for schizophrenia, all of whom reported hearing voices. Interviews with participants included questions about their voices’ identities, what those voices said and whether the patients conversed with their voices.
Among U.S. patients, 14 heard voices that told them to hurt other people or themselves and five described hearing voices as akin to being in a war or a battle. None of the patients reported predominantly positive voice-hearing experiences.
In India, 13 patients heard voices of kin or spouses offering guidance, scolding or giving commands to do household tasks. These voices were regarded as good, even if sometimes demanding or frightening. Only four people heard voices that regularly or occasionally commanded them to hurt someone.
In Ghana, 16 patients reported hearing God or another deity and 10 described voices that they heard as entirely or mostly positive. Others heard bad voices but insisted that good voices — usually God’s — were more powerful. Only two people said that voices told them to kill or to fight.
Most patients in each country, including the United States, were religious, so something else about participants’ backgrounds must have influenced the tendency to hear positive or negative voices, Luhrmann says.
Cultural differences in the new study help to explain why schizophrenia tends to be more severe and long-lasting in the United States than in India, Luhrmann proposes. Evidence on schizophrenia’s course in Ghana is too sparse for comparison.
The new findings lend support to a controversial treatment approach in the West, called the Hearing Voices movement, which for more than 20 years has taught people to interact with hallucinated voices as people. If this approach continues to catch on, a growing number of people with schizophrenia will become skilled at interacting constructively with their voices, Hopper predicts.