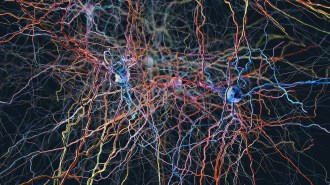
Breakdown of Alzheimer’s protein slows with age
Older brains clear out plaque-forming amyloid beta more slowly
- More than 2 years ago
A new study may help explain why Alzheimer’s is a disease of aging.
A protein fragment that forms the brain cell–killing plaques characteristic of Alzheimer’s disease sticks around longer and longer as people age, researchers report July 20 in the Annals of Neurology. That persistence may make it easier for plaques to form in older people, says study coauthor Randall Bateman, a neuroscientist at Washington University School of Medicine in St. Louis.
Bateman and colleagues measured how long it takes for the protein fragment known as amyloid beta, or A-beta, to be cleared from people’s brains. Some A-beta may be broken down and some may be transported out of the brain. For a 20-something-year-old, it takes about four hours for half of the A-beta in the brain to disappear. But that half-life increases to nearly 10 hours for people in their 80s, the researchers found.
“This particular finding is stunning,” says neurobiologist Caleb Finch of the University of Southern California in Los Angeles. Other researchers have collected evidence that it may be harder to break down many proteins with age. “This is the first [study] that I’m aware of to document it in the human brain,” Finch says.
Bateman and colleagues measured A-beta in cerebral spinal fluid collected hourly over 36 hours from study participants. How much A-beta appears in the fluid is an indicator of how much is getting flushed out or broken down in the brain. Participants included 100 people ages 60 to 87. About half had clinical signs of Alzheimer’s disease. Most of the people with signs of dementia also had amyloid plaques in their brains, while people who didn’t have Alzheimer’s tended not to have plaques. A separate group of younger, healthy people ages 30 to 59 were also analyzed. Over five decades of life, A-beta clearance slows by 60 percent, the researchers calculate.
Only average rates of A-beta turnover for groups of people were calculated in the study. Researchers would have to follow individuals over time to determine whether the process starts earlier for some people. A long-term study with many of the volunteers from this study is already under way, Bateman says. It will be years before the results are known.
Bateman’s team also examined what happens to the most worrisome form of A-beta, called A-beta42, in people with and without plaques. In people who didn’t yet have Alzheimer’s symptoms but already had plaques in their brains, A-beta42 appeared to get out of the brain faster than in people who didn’t have plaques. But Bateman and his colleagues don’t think that’s what is really happening. Instead, they suspect that A-beta42 is rapidly clumping into plaques and getting stuck in the brain.
A-beta42 clearance appears to slow again as people develop symptoms, the researchers discovered. That second slowdown may indicate the onset of the disease.
Aging brains may be able to cope with slowing decay rates until something happens to trigger plaque formation. The longer it takes to clear A-beta from the brain, the higher chance of pulling that trigger. Once plaque formation has started something else must change to cause the disease. “The question is,” says Bateman, “what changes?”
He and colleagues don’t yet know why A-beta turnover slows with age, or what the trigger for plaque formation might be. Nor is it clear that the changing A-beta42 half-life in people with plaques is associated with onset of the disease.