Bank voles provide clue to prion disease susceptibility
Mice engineered with vole protein suffer disorders that don’t usually infect them

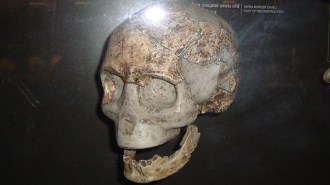
BLANK SLATE Bank voles carry a version of a normal protein that makes them particularly susceptible to prion diseases, such as mad cow disease.
Peter Trimming/Flickr (CC BY 2.0)
- More than 2 years ago
Prion diseases, the frightening neuron-killing disorders that transmit via infectious proteins rather than by viruses or bacteria, rarely jump from one species to another. But just a few amino acids can tear down the barriers that stop one animal from contracting another species’ prion disease.
Bank voles are particularly susceptible to the infectious brain-wasting diseases. That susceptibility stems from the structure of one of the vole’s brain proteins, researchers from the University of California, San Francisco report April 3 in PLOS Pathogens.
Prion diseases include mad cow disease in cattle, scrapie in sheep, chronic wasting disease in deer and several degenerative brain diseases in people, including Creutzfeldt-Jakob disease. They result when a normal brain protein called PrP twists into an abnormal shape known as a prion and remakes other PrP proteins in its disease-causing image. The misshapen proteins clump together and form plaques, killing brain cells in the process.
Normally, one animal’s prion has a hard time corrupting the PrP proteins from other species. That species barrier is higher for some species than for others. For instance, dogs and rabbits don’t get prion diseases under normal circumstances, says study coauthor Joel Watts, a neuroscientist at the University of Toronto.
But bank voles (Myodes glareolus), small mouselike rodents that live in woodlands in Europe and parts of Asia, “are susceptible to every prion disease known to man,” Watts says. That’s true when researchers inject prions directly into the rodents’ brains in the lab; no wild bank vole has ever been diagnosed with a prion disease, he adds.
Watts and his colleagues wondered if this susceptibility resulted from the vole’s physiology — perhaps the animal produces some other protein that helps contort PrP into the brain-killing form — or because of something special about the vole PrP protein itself.
To find out, Watts and his colleagues in Stanley Prusiner’s UCSF lab replaced the PrP protein in mice with the vole version. Researchers then injected infectious prions from any of eight species into the mice’s brains, and animals that produced high levels of vole PrP protein developed neurological diseases. Those results suggest that bank vole PrP is a “universal acceptor” that can adopt the infectious prion form from any species.
Exactly what gives the vole protein its mighty morphing abilities is a mystery. It differs from the normal mouse PrP by only eight amino acids, and, Watts says, “none of them grab you and make you say: Ah! That’s it!”
Mice making high levels of their own PrP are only marginally susceptible to other species’ prion diseases and sometimes don’t contract them at all, Watts says. But mice bearing the vole version of PrP developed prion diseases surprisingly quickly, says David Westaway, a neuroscientist a the University of Alberta in Edmonton, Canada. “That’s a logistical advantage” for researchers studying prion diseases, he says, because it could speed up experiments by months or years and accelerate work toward potential therapies.
“The idea that bank vole PrP might be a ‘universal acceptor’ could be significant for both scientific and practical reasons,” says Surachai Supattapone, a biochemist at the Dartmouth College’s medical school. If prions from any species can really wrench the vole PrP into disease-causing states, researchers could test whether a new neurological disease is a prion disease by injecting brain matter from sick animals into mice carrying the vole proteins. If the mice then develop the disease, there’s a good chance it’s caused by a prion, he suggests.
Such a test would have been useful at the beginning of the mad cow or chronic wasting disease outbreaks, he says. “It would also be useful to detect and study potential cases of prion disease in unusual species, such as zoo animals.”