Transplant Hope: New thymus tissue jump-starts immune system in babies
Babies born without a thymus gland–and therefore bereft of a functioning immune system–are easy prey for disease-causing invaders. If untreated, this deficiency, called severe DiGeorge syndrome, is invariably fatal before a child’s third birthday.
For babies with the syndrome, also called DiGeorge anomaly, a thymus transplant may present a life-changing option. But scientific information on such transplants has been limited to the results of sporadic case studies because the disease is rare, affecting only a handful of newborns each year in the United States. Researchers at Duke University Medical Center in Durham, N.C., now report the largest series of thymus transplants–in 12 children with DiGeorge syndrome over 8 years–and show success in establishing an immune system in many of these babies. The report appears in the Aug. 1 issue of Blood.
The babies received transplanted thymus tissue within their first few months of life. The grafted tissue takes a long time to build up a protective army of white blood cells called T cells, says M. Louise Markert, a pediatric immunologist at Duke, so the children remained especially vulnerable to infections for months after the surgery.
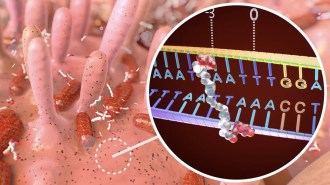
White blood cells begin in the bone marrow. Some of these migrate to the thymus gland, which sits above the heart, and there become T cells. Named for the thymus gland, T cells are frontline defenders in the immune system and champs at distinguishing the body’s own tissues from foreign materials.
For the transplants, doctors salvaged some thymus tissue that otherwise would have been discarded from children undergoing heart surgery. The material was nourished in a lab dish, where the team removed existing T cells to keep them from attacking the babies who subsequently received the tissue. The doctors then implanted the thymus tissue into the recipients’ thigh muscles.
Despite the transplant, five of the babies died within 5 months of surgery from infections and brain hemorrhages that were complications of DiGeorge syndrome, Markert reports. These deaths weren’t caused by the transplants, she says.
Of the seven surviving children, all are free of infection and living at home. The children got their transplants between 1993 and 2001, and they now average 4 years since the surgery. Some of the older ones attend elementary school, Markert says.
While some of the children still have diminished hearing, mild mental retardation, and difficulty swallowing–all common to DiGeorge patients–the children are fending off infections, Markert says.
T cell concentrations in the children’s blood are slightly below normal but not dangerously so, she adds. Three children tested 2 years after transplantation were all making antibodies, another good sign. In all seven children, the immune deficiency appears to be corrected, she concludes.
“This is a really scholarly piece of work,” says Richard Hong, an immunologist at the University of Vermont in Burlington. Other scientists have investigated use of transplants of mature T cells for DiGeorge patients, but the Duke study validates thymus transplantation as the best treatment, he says.
****************
If you have a comment on this article that you would like considered for publication in Science News, send it to editors@sciencenews.org. Please include your name and location.