Genes that control toxin production in C. difficile ID’d
New finding could lead to better ways to disarm gut-wrenching superbug
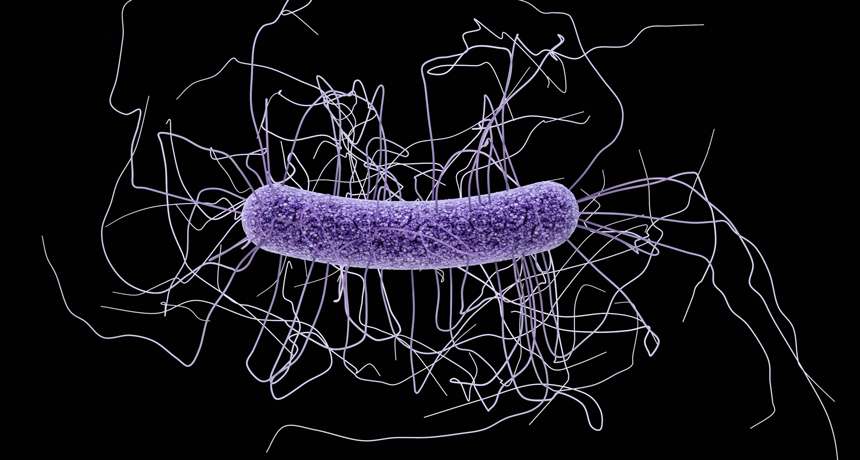
BATTLING A BUG Unraveling the toxin-making genetic pathway in Clostridium difficile (shown) may help scientists design nonantibiotic therapies to fight the superbug.
James Archer/CDC
- More than 2 years ago
A new genetic discovery could equip researchers to fight a superbug by stripping it of its power rather than killing it outright.
Scientists have identified a set of genes in Clostridium difficile that turns on its production of toxins. Those toxins can damage intestinal cells, leading to diarrhea, abdominal pain and potentially life-threatening disease. Unlocking the bug’s genetic weapon-making secret could pave the way for new nonantibiotic therapies to disarm the superbug while avoiding collateral damage to other “good” gut bacteria, researchers report August 16 in mBio.
Identifying a specific set of genes that control toxin production is a big step forward, says Matthew Bogyo. Bogyo, a chemical biologist at Stanford University, also studies ways to defuse C. difficile’s toxin-making.
C. difficile bacteria infect a half million people and kill about 29,000 each year in the United States. In some individuals, though, the microbe hangs out in the gut for years without causing trouble. That’s because human intestines normally have plenty of good bacteria to keep disease-causing ones in check. However, a round of antibiotics can throw the system off balance, and if enough good bugs die off, “C. difficile takes over,” says lead author Charles Darkoh, a molecular microbiologist at the University of Texas Health Science Center at Houston. As infection rages, C. difficile can develop resistance to antibiotic drugs, turning it into an intractable superbug.
Darkoh’s team reported last year that C. difficile regulates toxin production with quorum sensing — a system that lets bacteria conserve resources and launch an attack only if their numbers reach a critical threshold. That study identified two sets of quorum-signaling genes, agr1 and agr2, that could potentially activate toxin production.
In the new analysis, Darkoh and colleagues tested the ability of a series of C. difficile strains to make toxins when incubated with human skin cells. Some C. difficile strains had either agr1 or agr2 deleted; others had all their quorum-sensing genes or lacked both gene sets. Agr1 is responsible for packing the superbug’s punch, the researchers found. C. difficile mutants without that set of genes made no detectable toxins, and skin cells growing in close quarters stayed healthy. Feeding those mutant bugs to mice caused no harm, whereas mice that swallowed normal C. difficile lost weight and developed diarrhea within days. In the skin cell cultures, agr2-deficient strains were just as lethal as normal C. difficile, showing that only agr1 is essential for toxin production.
Based on their new findings, Darkoh and colleagues have identified several compounds that inactivate C. difficile toxins or block key steps in the molecular pathway controlling their production. The researchers are testing these agents in mice.
In a mouse study published in Science Translational Medicine last year, Bogyo and colleagues found a different compound that could disarm C. difficile by targeting its toxins. And several companies are trying to fight C. difficile with probiotics — cocktails of good bacteria. Results have been mixed.